Understanding the Root Canal Procedure: What You Need to Know
Root canals can be an intimidating concept for many people, often associated with pain and discomfort. However, advancements in dental technology and anesthetic techniques have made the root canal procedure far more manageable than it once was. In fact, it’s one of the most common and effective treatments to save a tooth from extraction. In this guide, we’ll take an in-depth look at the root canal procedure, helping you understand what to expect, why it’s needed, and how it benefits your oral health.
What is a Root Canal?
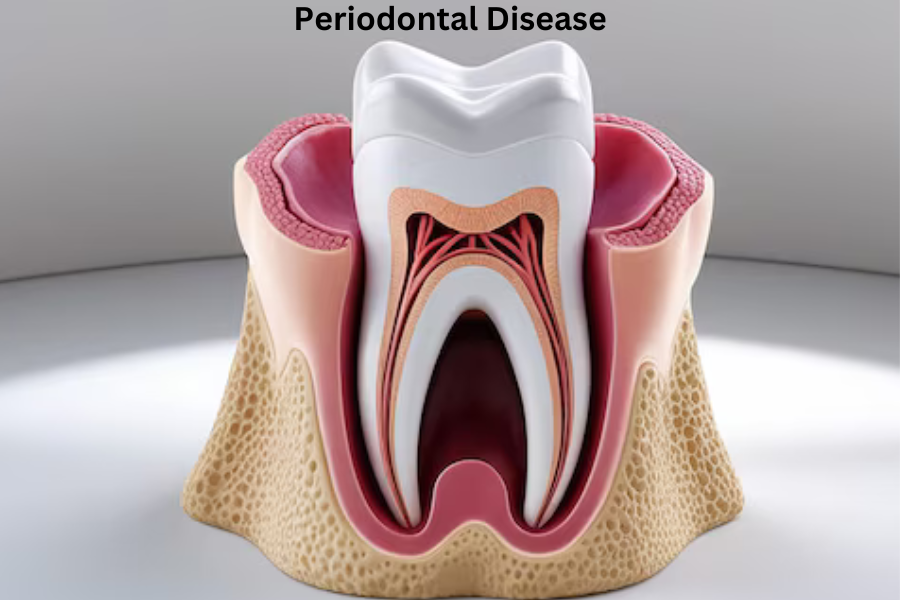
A root canal is a dental procedure used to treat an infected or damaged tooth. The goal is to remove the infected pulp tissue inside the tooth, clean the canals, and seal the area to prevent further infection. The term “root canal” refers to the natural cavity within the center of the tooth that contains the pulp, which consists of nerves, blood vessels, and connective tissue. When this pulp becomes infected or inflamed, usually due to deep decay, repeated dental procedures, or trauma, a root canal becomes necessary to save the tooth.
Signs You May Need a Root Canal
You might wonder how to determine whether you need a root canal. There are several symptoms that could indicate that your tooth is infected or damaged. Some common signs include:
- Severe Tooth Pain: Persistent pain, especially when chewing or applying pressure, could be a sign of an infection within the tooth.
- Prolonged Sensitivity: If you experience prolonged sensitivity to hot or cold temperatures, it may suggest that the pulp inside your tooth is damaged.
- Swollen Gums: Swelling around the affected tooth or the presence of a bump (abscess) on the gums can indicate infection.
- Discoloration: A tooth that becomes darker in color may be dying or dead due to damage to the pulp.
- Cracked or Chipped Tooth: Physical trauma to a tooth can cause damage to the pulp and may require a root canal.
It’s important to consult with a dentist if you experience any of these symptoms, as early detection and treatment can save your tooth.
Why is a Root Canal Necessary?
The root canal procedure is essential when the pulp inside a tooth becomes infected or inflamed. If left untreated, the infection can spread to surrounding tissues, leading to abscess formation, bone loss, and even the loss of the tooth itself. Additionally, the infection could enter the bloodstream and cause systemic health issues.
Root canals not only preserve the tooth but also relieve pain, improve overall oral health, and prevent future complications.
The Root Canal Procedure: Step-by-Step
Now that we’ve covered what a root canal is and why it’s necessary, let’s dive into the steps involved in the procedure itself. Understanding the process can help alleviate some of the fear or anxiety associated with the treatment.
- Diagnosis and X-rays
Before the procedure begins, your dentist or endodontist (a specialist in root canals) will take X-rays to examine the tooth’s condition and to determine the extent of the infection or damage. This step is crucial for planning the treatment and ensuring that the root canal addresses the full scope of the problem.
- Administering Local Anesthesia
One of the biggest concerns people have about root canals is pain. However, thanks to modern anesthesia, the procedure is typically no more painful than getting a filling. Your dentist will administer a local anesthetic to numb the affected tooth and surrounding area. This ensures you remain comfortable and pain-free throughout the treatment.
- Placing a Dental Dam
To isolate the tooth and keep the area clean during the procedure, a rubber dam (a small sheet) will be placed over the tooth. This helps prevent saliva and bacteria from entering the tooth while it’s being treated.
- Accessing the Pulp Chamber
Once the area is numb, the dentist will create a small opening in the top of the tooth to access the pulp chamber. This allows them to remove the infected or inflamed pulp from inside the tooth and root canals.
- Cleaning and Shaping the Canals
Using specialized dental instruments, the dentist will carefully clean out the infected tissue from inside the tooth. The root canals are then shaped and disinfected to remove any lingering bacteria or debris. This step is crucial in preventing reinfection.
- Filling the Canals
After the cleaning process is complete, the dentist will fill the canals with a biocompatible material called gutta-percha. This rubber-like substance seals the space and prevents bacteria from re-entering the tooth. In most cases, a temporary filling is placed on top to protect the tooth until a permanent restoration is applied.
- Restoring the Tooth
In the weeks following the procedure, you’ll return to your dentist to have a permanent dental crown or filling placed on the treated tooth. This final step is critical because it reinforces the tooth’s structure, protecting it from fractures and further damage. A crown is typically recommended for molars, as they bear the brunt of chewing forces.
What to Expect After the Procedure
After your root canal, it’s normal to experience some mild discomfort or sensitivity for a few days. This can usually be managed with over-the-counter pain relievers like ibuprofen or acetaminophen. In most cases, patients can return to their normal activities within a day or two.
If you experience severe pain, swelling, or signs of infection after the procedure, you should contact your dentist immediately.
Benefits of a Root Canal
Root canals offer numerous benefits for your oral health. Here are some of the most important ones:
- Pain Relief: One of the primary reasons for undergoing a root canal is to alleviate the pain caused by infection or inflammation in the pulp.
- Tooth Preservation: Root canals save natural teeth, preventing the need for extraction and costly tooth replacement options such as dental implants or bridges.
- Preventing Infection Spread: By removing the infected tissue, root canals help prevent the spread of infection to other teeth and the surrounding gum tissue.
- Improved Function: A restored tooth functions just like a natural tooth, allowing you to chew, bite, and speak normally.
Root Canal Alternatives
In some cases, a root canal may not be possible or recommended. The alternative to a root canal is tooth extraction. However, removing the tooth leads to other issues, such as a gap in your smile, difficulty chewing, and shifting teeth. Extraction should generally be considered a last resort, as saving the natural tooth is usually the best option for long-term oral health.
If extraction is necessary, your dentist will discuss tooth replacement options, such as dental implants, bridges, or dentures, to restore function and appearance.
Myths About Root Canals
Despite their benefits, root canals are surrounded by myths and misconceptions. Let’s address a few common ones:
- Myth: Root canals are extremely painful.
Reality: The procedure is no more painful than getting a filling, thanks to local anesthesia. In fact, it often relieves the pain caused by the infection.
- Myth: Root canals cause illness.
Reality: This myth stems from outdated information. Modern root canals are safe, and there’s no scientific evidence linking them to illness elsewhere in the body.
- Myth: Extraction is better than a root canal.
Reality: Keeping your natural tooth is preferable to extraction, as it preserves the structure of your jaw and prevents other dental problems.
Conclusion
Understanding the root canal procedure can go a long way in easing anxiety about the treatment. While the process may seem complex, it’s a routine dental procedure that effectively addresses tooth infections, relieves pain, and preserves your natural teeth. If you’re experiencing symptoms of an infected or damaged tooth, consult your dentist to determine whether a root canal is the right option for you.